Primary Care First (PCF), a new care delivery and payment model from the CMS Innovation Center is another approach to advancing primary care. PCF eligibility and care delivery design mirror the CPC+ model in several ways, but is distinct in others. The model leverages both population-based and flat fee visit payments to promote access and better care delivery. The impact of this approach to payment is expected to vary based on practice characteristics such as beneficiary risk profile.
On October 24, 2019, the Centers for Medicare and Medicaid Services (CMS) and the CMS Innovation Center posted a request for applications (RFA) for Primary Care First (PCF). Initially announced in April 2019, PCF represents the next step in the evolution of the CMS Innovation Center’s advanced primary care model portfolio. Applications for 2021 are due January 22, 2020.
Trump Administration Adheres to Key Themes with New Delivery Model Applications
US Department of Health and Human Services Secretary Alex Azar has outlined four departmental priorities: the opioid crisis, drug pricing, health insurance reform and value-based care. Within the value-based care bucket, the Administration has focused on pioneering bold new models in Medicare and Medicaid. Through requests for information, regulatory changes and new payment models, themes that define this Administration’s value-based payment agenda have emerged:
- Shifting risk from the federal government to providers and other entities at a local level;
- Engaging and empowering beneficiaries; and
- Reducing administrative burdens.
PCF adheres to these themes, introducing new elements and building on the lessons learned from previous Innovation Center models.
Primary Care First
Building on the Comprehensive Primary Care initiative and Comprehensive Primary Care Plus (CPC+), PCF is intended to test whether advanced primary care can reduce total cost of care while improving or maintaining quality. The model is designed for primary care practices with advanced primary care capabilities, including those specializing in caring for complex, chronically ill patient populations.
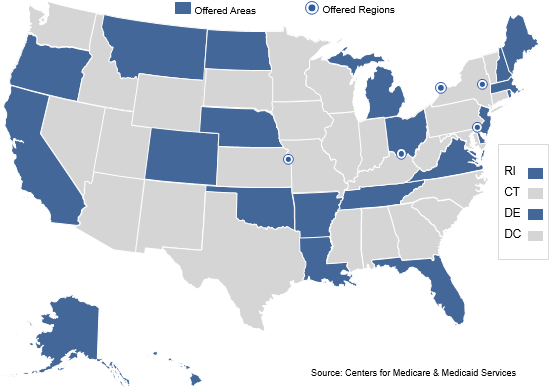
The model will be tested over a six-year period, with one cohort participating from 2021 through 2025 and a second participating from 2022 through 2026. Practices located in the 26 eligible PCF regions that are not currently participating in CPC+ are eligible to participate in the first cohort. The second cohort will consist only of current CPC+ practices.
Like CPC+, PCF is a multi-payer model. CMS will encourage Medicare Advantage, commercial and Medicaid plans as well as state Medicaid agencies to engage practices on similar outcomes with respect to their members. Payers have the option to submit a non-binding Statement of Interest signaling their interest in partnering in PCF. The formal payer solicitation period will open December 9, 2019, and close March 13, 2020.
Payers that want to participate in this model must commit to pursuing private payment arrangements and to using at least a partial alternative to FFS payment, such as a population-based payment, and must offer an opportunity for a performance-based incentive payment that aligns with the PCF financial model.
Practice and payer selections are currently scheduled to take place in winter/spring 2020.
PCF Eligibility and Care Delivery Design
PCF Eligible Participating Practices
To participate in PCF, practices must meet certain criteria:
- Have at least 125 attributed beneficiaries;
- Achieve thresholds for primary care billing based on revenue;
- Have experience with value-based payment arrangements or payments based on quality, cost and/or utilization performance;
- Use 2015 CEHRT, support data exchange with other providers and health systems via Application Programming Interface, and agree to connect to their regional health information exchange; and
- Participate in one of 26 selected regions.[1]
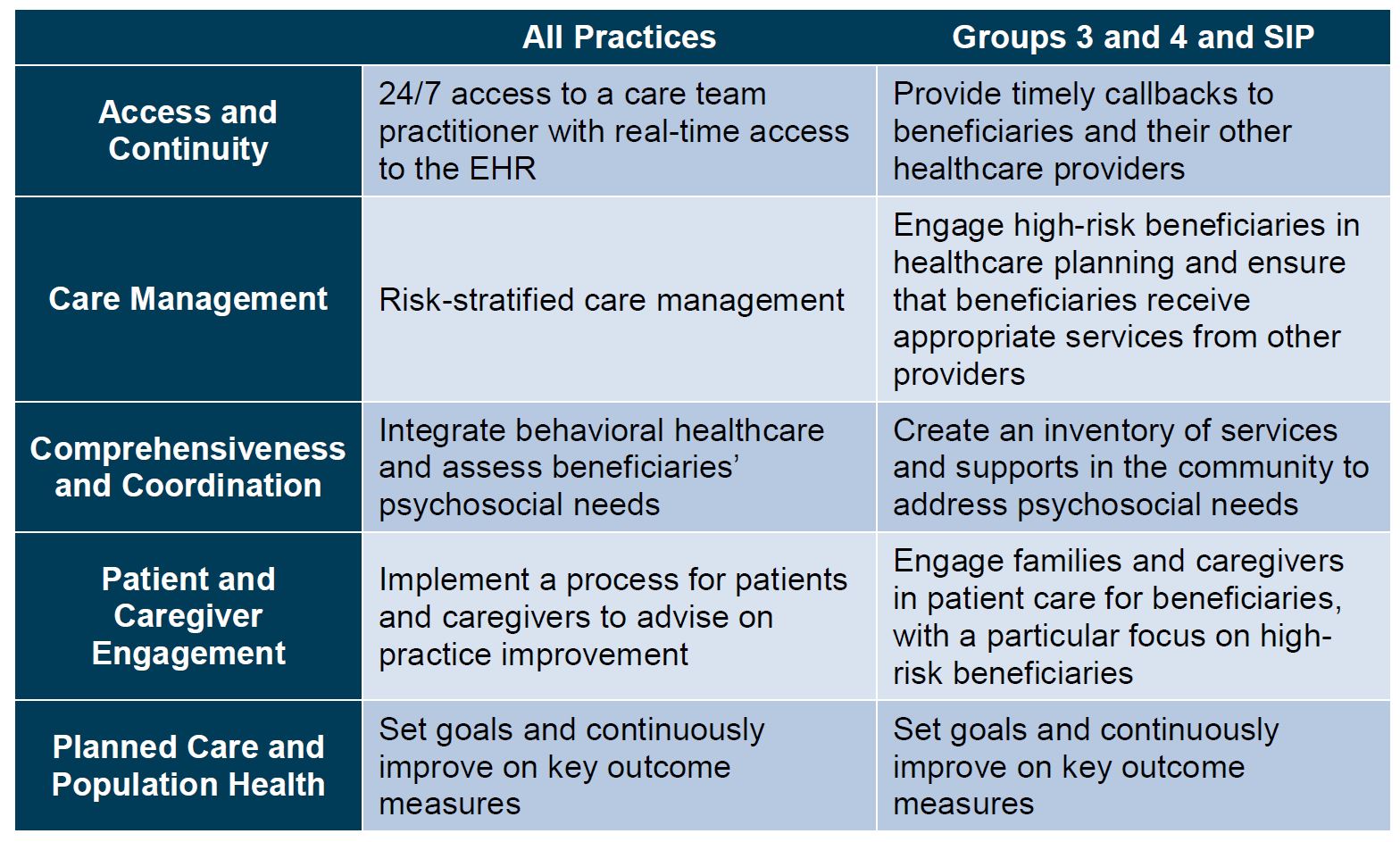
Care Delivery Design Elements
PCF primary care practitioners are incentivized to achieve better care at a lower cost by delivering on five primary care functions:
Empowering Beneficiary Choice
PCF includes voluntary alignment, allowing a beneficiary to be assigned to a PCF practice by attesting to her choice of a primary care practitioner through MyMedicare.gov. Attestation will supersede future claims-based attribution to most other Innovation Center models or PCF. PCF will also include claims-based attribution as a second step.
Seriously Ill Population Component
The seriously ill population (SIP) component of PCF is designed to support an intensive, time-limited intervention for seriously ill beneficiaries who lack care management in FFS Medicare. The SIP option provides a time-limited enhanced payment until the beneficiary is stabilized and transitioned out of the SIP component. SIP practices will not be required to meet all of the thresholds and requirements described in the PCF option above, but will be required to demonstrate advanced competencies and clinical abilities to manage the population. CMS will encourage SIP component participants to maintain an eight-month annual average length of attribution. The SIP option can be a standalone option or combined with PCF.
In the SIP option, the primary care practice will designate a geographic service area, and CMS will assign SIP beneficiaries based on geographic proximity within that service area. Once a beneficiary indicates interest, CMS will provide his contact information to the practice and the practice will have 60 days to engage the beneficiary. After the practice submits a claim for the first face-to-face visit, the SIP beneficiary will be attributed and the monthly payments will begin. CMS will also identify non-claims-based clinical criteria that beneficiaries must meet to be eligible for direct referral.
CMS will make a one-time payment of $325 after the practice has the first face-to-face visit with the beneficiary. Following the first visit, the practice will receive a $275 per-beneficiary per-month (PBPM) base rate minus a $50 withhold until the end of the performance year to ensure minimum quality standards are achieved.
PCF Payment Design and Impact
The payment structure for PCF has multiple elements:
- Total Primary Care Payment (TPCP). This consists of a lump sum professional population-based payment (PBP) with a base rate ranging from $28 to $175 determined using average risk scores for the practice and a flat $40.82 base rate per-visit primary care fee. The TPCP will include geographic adjustment, risk adjustments[2] and a leakage reduction that will account for the number of primary care services attributed beneficiaries receive outside of the PCF practice.
- Performance-Based Adjustment (PBA). Beginning in performance year two, the TPCP will be adjusted based on performance on quality and patient experience and a measure of acute hospital utilization. Practices will be required to meet certain performance standards and will receive positive, negative or neutral PBAs. Practices will receive a maximum possible positive adjustment of 50% and maximum possible negative adjustment of -10%. The PBA has a regional performance bonus and a continuous improvement bonus.
Although the precise impact of the PCF payment methodology is difficult to predict, the CMS Innovation Center provided sufficient detail to allow evaluation of the impact of various payment levers. Below we examine individual elements of the methodology and how they affect PCF payments.
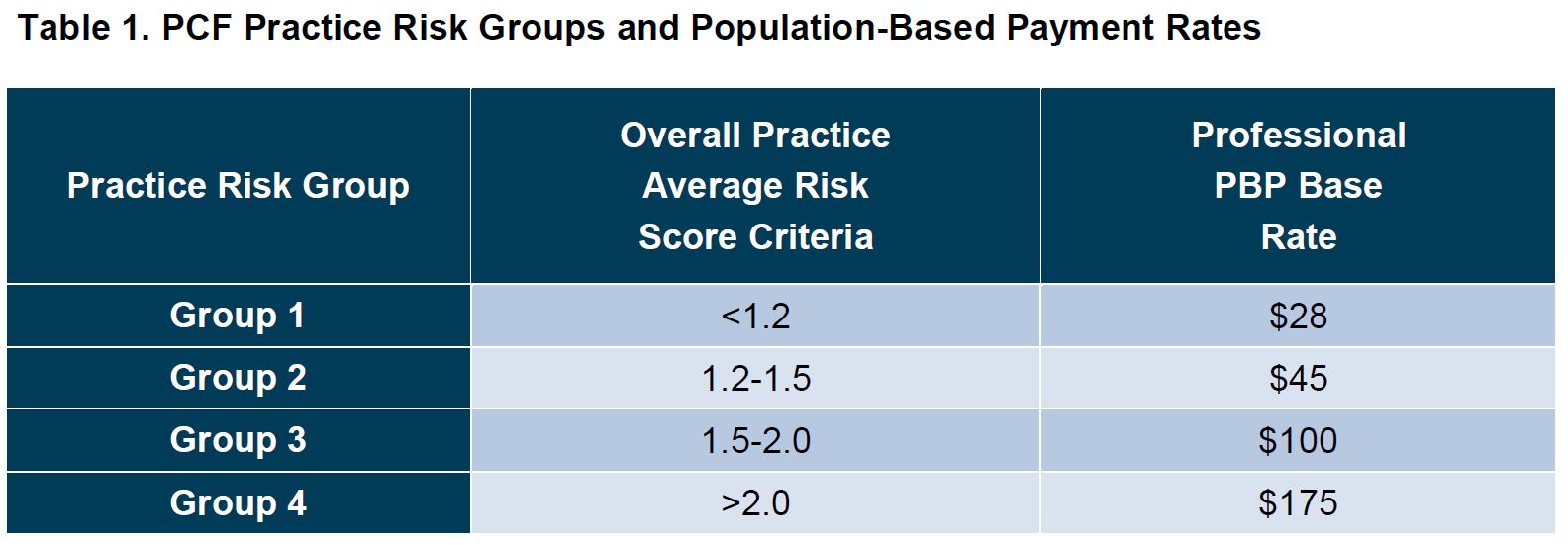
Population-Based Payments and Practice Average Risk Score
Under the PCF payment methodology, the monthly PBP is determined based on each participating practice’s average risk score. The higher the risk score, the higher the PBP (Table 1).
The CMS Innovation Center has not yet released its final risk adjustment methodology. The risk adjustment will be based on hierarchical condition categories (HCCs).
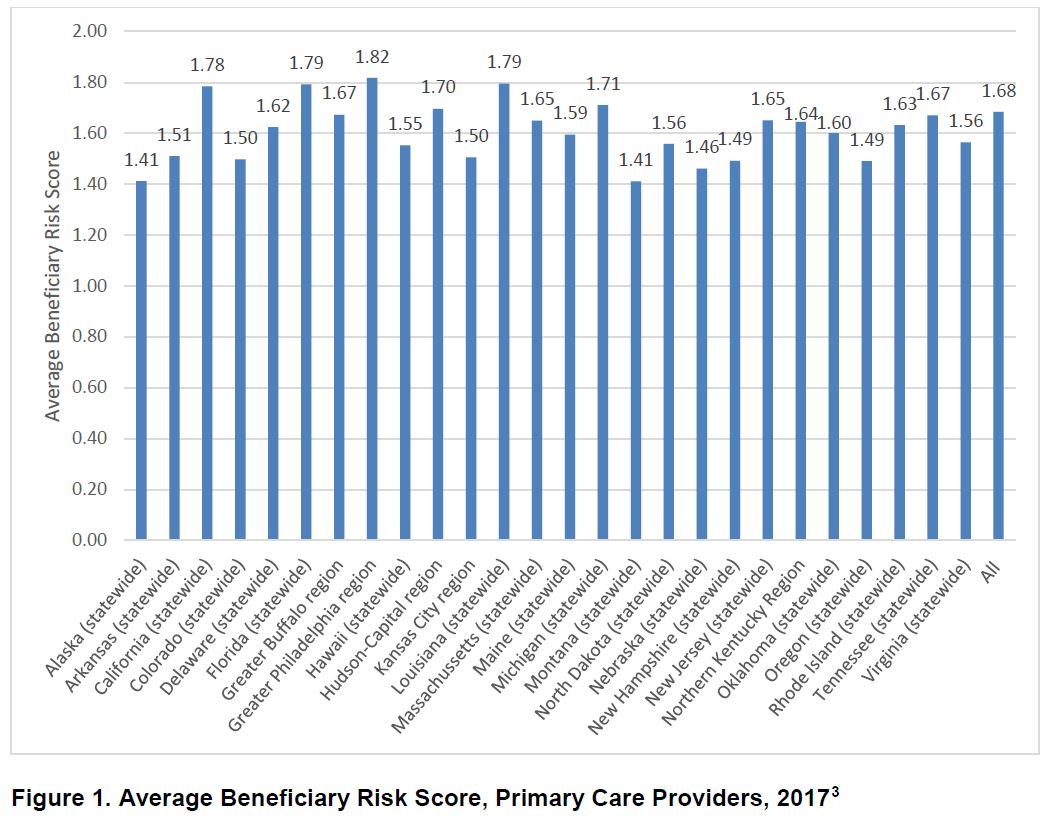
Using the 2017 Medicare Physician and Other Supplier Public Use File, an examination of primary care provider beneficiary HCC risk scores across the 26 PCF regions indicates regional variation (Figure 1).
The lowest average beneficiary risk scores for primary care providers were in Alaska and Montana (1.41), while the highest average risk score was in the Greater Philadelphia Region (1.82). Average beneficiary risk scores are also likely to vary from practice to practice.
Still, data suggest that the majority of PCF practices are likely to receive either a $45 (group 2) or a $100 (group 3) unadjusted PBPM rate[4]. Final PBP payments will be adjusted to account for leakage (i.e., primary care services that attributed beneficiaries receive outside of the PCF practice).
Table 2 illustrates how annual PBP payments might vary based on risk score and leakage for a PCF practice with 200 attributed beneficiaries.
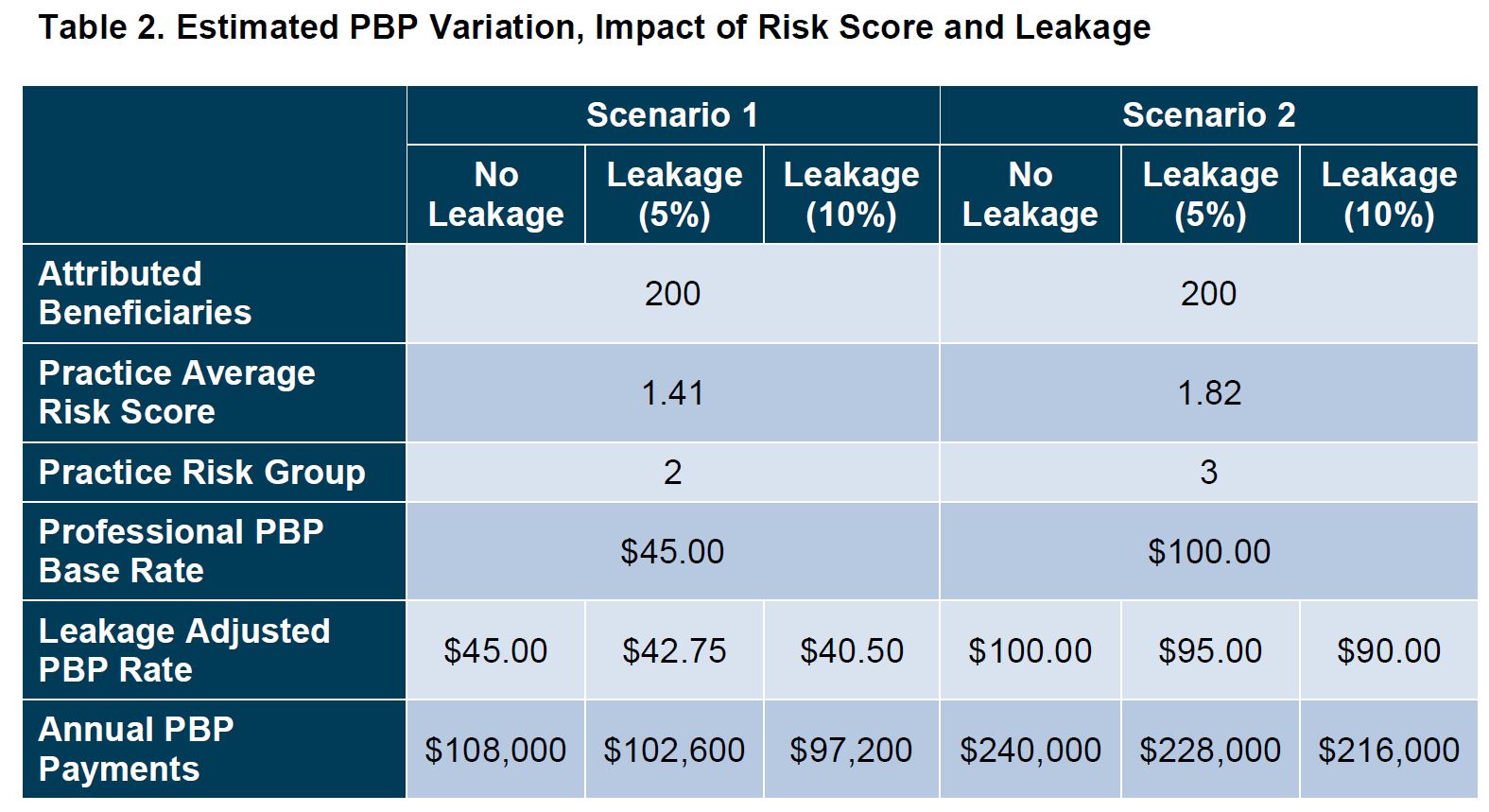
PCF practices in higher risk groups will be affected more by the leakage reductions. For PCF practices in risk group 4, the PBP will be reduced by $1.75 for every percent increase in the leakage reduction. In contrast, PCF practices in risk groups 3, 2 and 1 will lose $1.00, $0.45 and $0.28 for every percent increase. Table 3 shows the impact of these adjustments on a PCF practice with 200 attributed beneficiaries across practice risk groups.
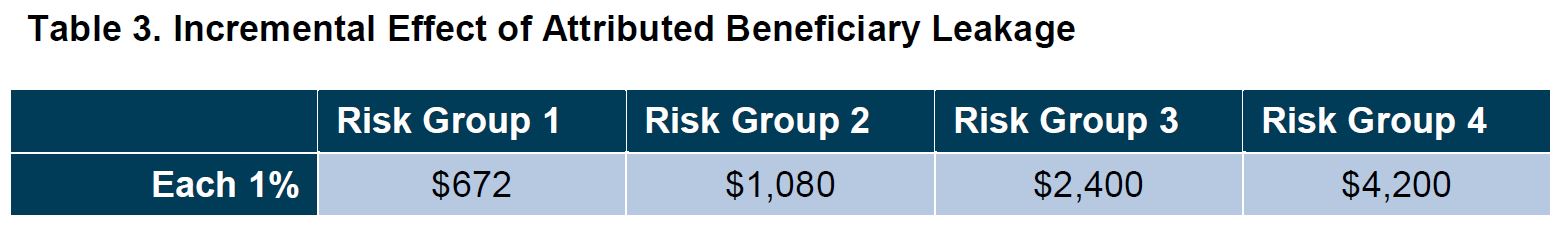
As leakage increases, so do the negative payment effects. To maximize payment under the PCF, controlling leakage will be important—especially for large, high-risk practices.
Flat Visit Fee and the Distribution and Volume of Primary Care Services
With a shift towards a flat fee payment for a broad range of primary care services, the number and type of services provided by PCF practices will also influence how they fare financially under the model.
An analysis of primary care services provided by primary care providers across the 26 PCF regions indicates that across this group, the majority of services provided are level 3 and level 4 evaluation and management services.[5] Level 3, level 4 and level 5 established patient evaluation and management services comprised 80% of the primary care services provided (Figure 2).
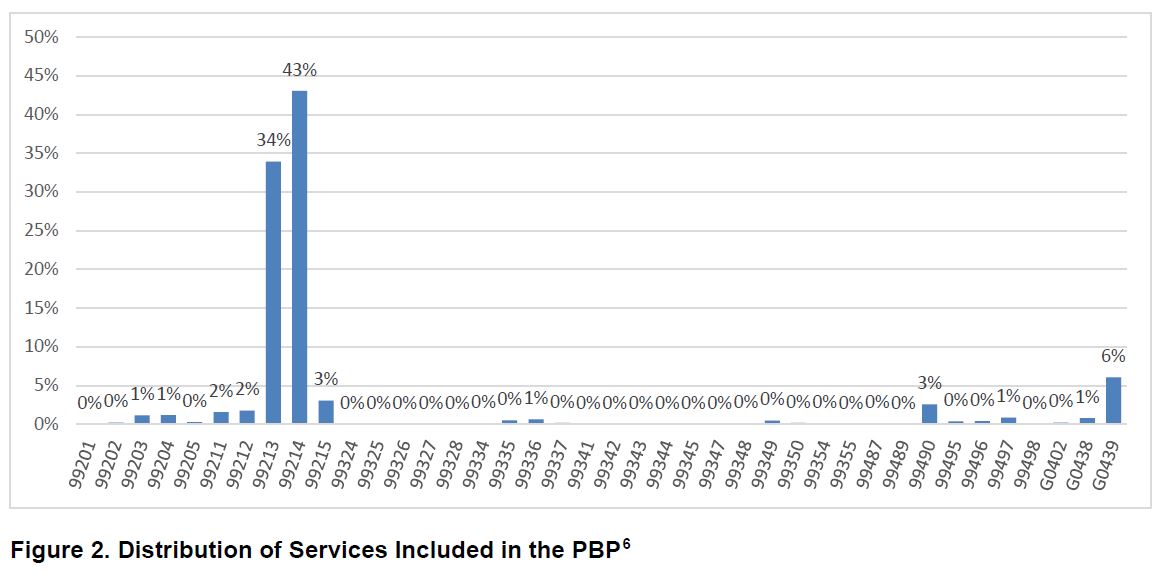
Figure 2. Distribution of Services Included in the PBP[6]
Types and distribution of services vary from practice to practice, but the distribution of services shown in Figure 2 is a helpful benchmark for understanding the potential impact of the PCF flat visit fee.
Table 4 models out the per-visit impact of the flat visit fee on a PCF practice whose services mirror the distribution shown in Figure 2.
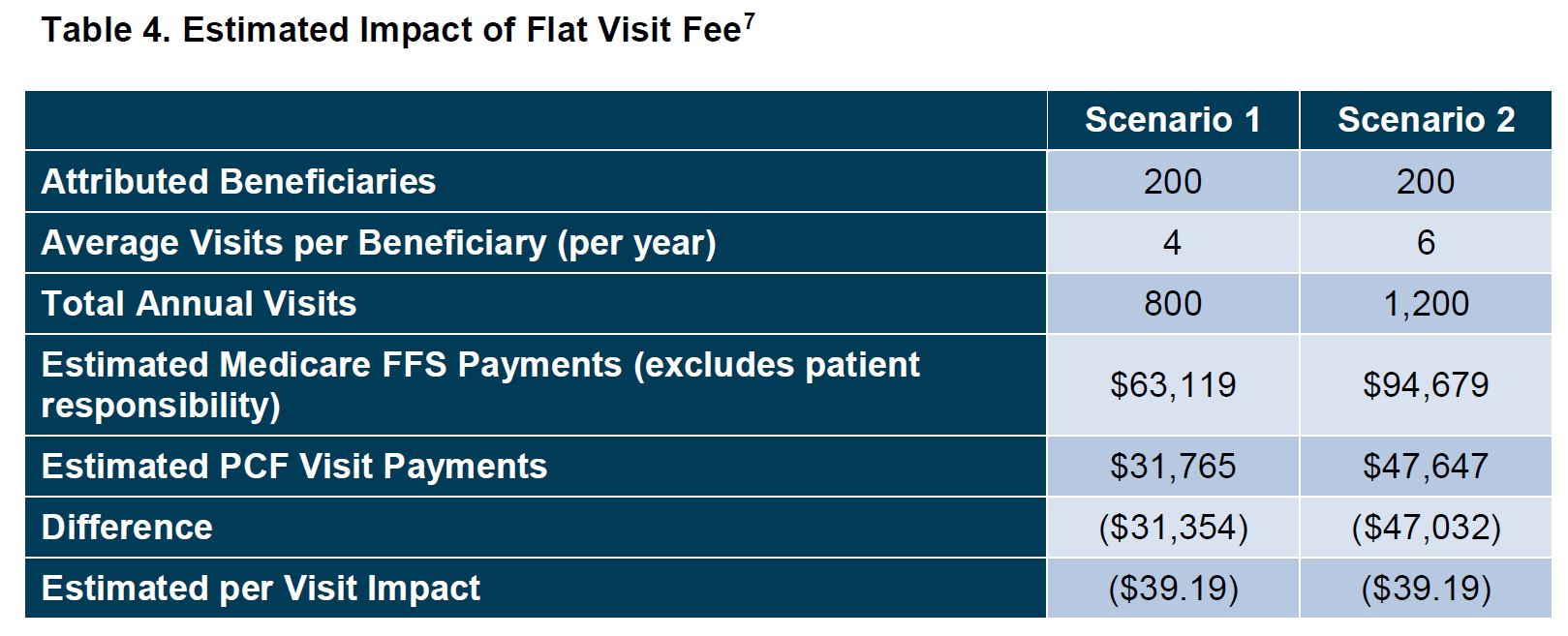
The impact of the flat visit fee does not change based on volume. However, changes to the distribution of services will alter the per-visit impact. For high-risk practices that provide more level 4 and level 5 visits, the loss per visit will increase under the model.
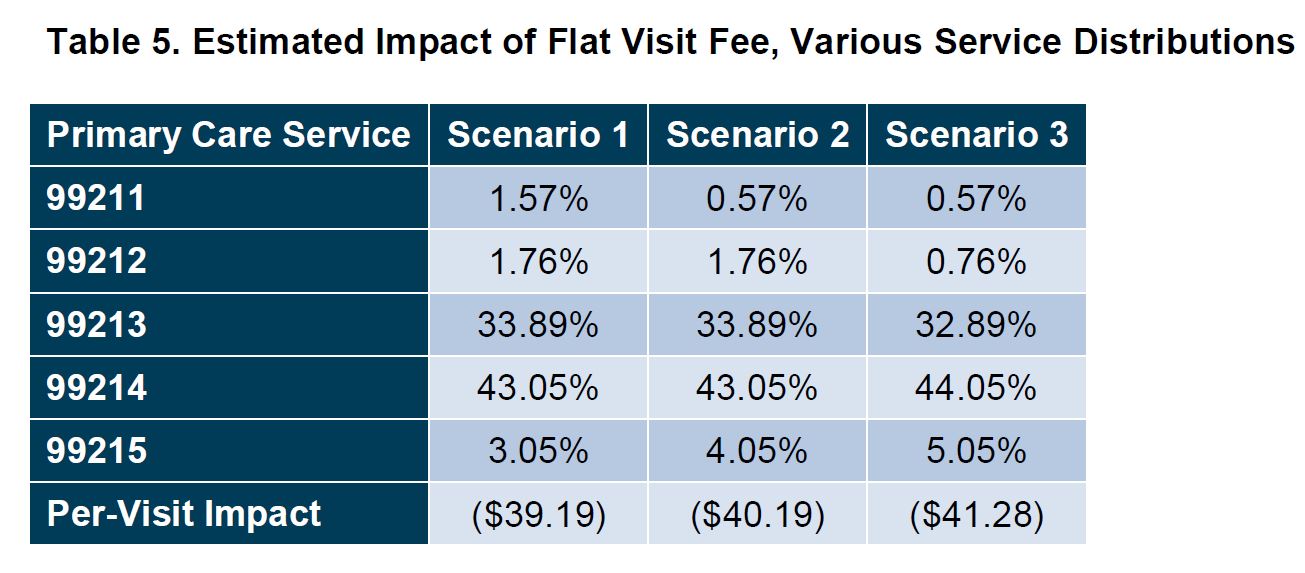
These estimates reflect Medicare FFS payment rates. Medicare recently finalized changes to payment for evaluation and management services, which will alter the estimated per-visit impact. Because those changes increase payment for most evaluation and management services, the per-visit loss will likely be greater than shown in Table 5.
TPCP – Putting It All Together
The PCF is intended to incentivize delivery of better care, and the established TPCP structure is intended to support that goal. Practices may use monthly PBP payments to support non-traditional services that help deliver better care. However, the value of PBP payments is reduced by the flat visit fee, which results in less payment for care delivered. Table 6 below shows the net value of TPCP payments.
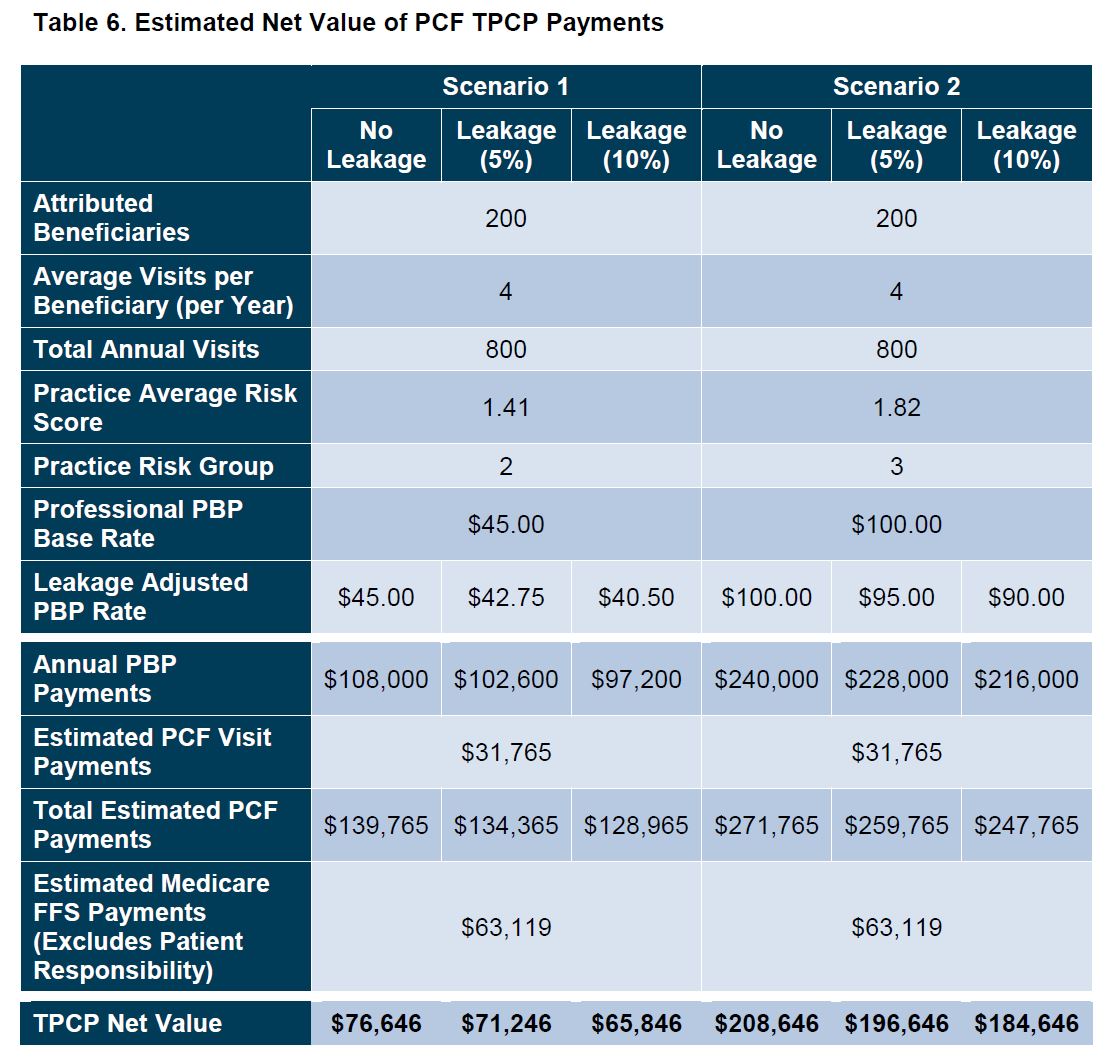
The net value of TPCP is clearly greater for high-risk practices. High-risk practices will have greater funds available to invest in non-traditional services to support better care delivery.
As the program proceeds, it will be important to understand whether the CMS Innovation Center’s risk adjustment methodology accurately captures beneficiary risk. If it does not, PCF practices assigned to the lower risk groups (e.g., groups 1 and 2) may not be able to enhance care delivery to the same extent as practices assigned to higher risk groups (e.g., groups 3 and 4) and PCF results may be misleading.
Performance-Based Adjustment
Finally, although not modeled here, the net value of TPCP will be increased or decreased based on PCF practice performance and the applicable PBA. Losses are limited to 10%. Any reduction in payment as a result of the PBA will further reduce the net value of the TPCP.
Application Deadline
Applications for 2021 are due January 22, 2020.
[1] Practices participating in Independence at Home (IAH) are eligible for the first cohort of PCF even if PCF is not offered in their region(s). IAH is currently scheduled to end December 31, 2020. If it is extended, CMS may reconsider this approach.
[2] CMS indicates that the risk adjustment methodology will be announced separately at a later date.
[3] 2017 Medicare Physician and Other Supplier Public Use File.
[4] CMS will pay the PBP quarterly on a prospective basis, but it is calculated based on a PBPM rate.
[5] 2017 Medicare Physician and Other Supplier Public Use File.
[6] Although all of these services are included in the PBP, not all are included in the flat visit fee. Chronic Care Management services (99487, 99489–99491) are excluded from the flat visit fee. Practically, this means that under PCF, these services are not reimbursed (payment is presumed to be part of the PBP).
[7] The analysis does not include geographic adjustment. However, both Medicare FFS and PCF Visit payments are geographically adjusted. We have also excluded patient coinsurance from the analysis. If a PCF practice elects to waive coinsurance or charge a flat fee (e.g., $10 copay), this would increase the per-visit impact.





 />i
/>i

